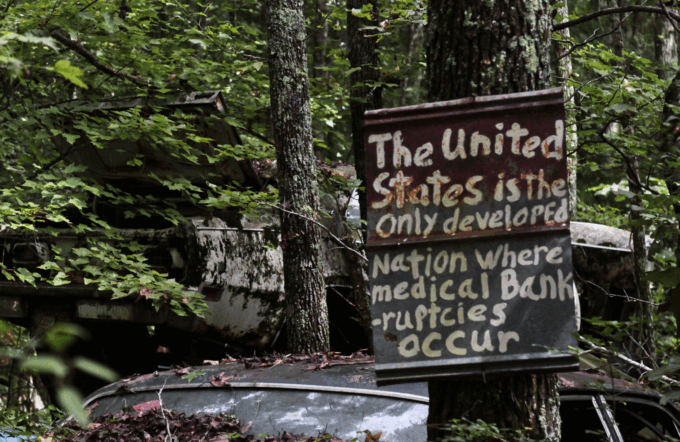
Photo by Chela B.
On October 7, House Democrats introduced a bill – Seniors Deserve SMARTER (Streamlined Medical Approvals for Timely, Efficient Recovery) Care Act – to repeal the WISeR model, scheduled to be implemented on January 1, 2026 by the Centers for Medicare and Medicaid (CMS). It is, in short, an effort to reverse a policy move that would enrich private AI contractors and hurt Medicare patients.
The WISeR model – intended to reduce spending on seniors in traditional Medicare through Wasteful and Inappropriate Service Reduction – will require prior authorization in traditional Medicare for a set of health services and will use AI (artificial intelligence) in making the determination to authorize or deny care. We already know what is likely to occur. Preauthorization in Medicare Advantage (MA), where it is widely used to manage utilization of health services, has led to millions of seniors being denied necessary care. In contrast, traditional Medicare only uses preauthorization in very limited circumstances.
In 2023, MA providers filed around 50 million prior authorization requests for enrollees, with insurance companies denying around 3.2 million (6.4 percent). Nearly 82 percent of denied requests were overturned on appeal, pointing to patients being denied necessary medical treatments. However, patients and providers appealed denials only 11.7 percent of the time, allowing providers toprofit from denying care to millions of seniors.
The pilot project, which will be rolled out in six states — Arizona, New Jersey, Ohio, Oklahoma, Texas and Washington — will use contractors to provide preauthorization for the procedures for Medicare recipients. The contractors will earn 10 to 20 percent of the savings they generate, giving them a financial incentive to deny necessary care. The more they deny, the more money they earn.
The contractors selected for this were chosen for their ability to test the use of AI to approve or deny preauthorization requests. In Texas, the contractor is Cohere, an AI prior authorization and clinical intelligence company. In Oklahoma, it is Humata, a new health technology start up founded two years ago by a Mayo Clinic radiologist. In New Jersey, the contractor is Genzeon, a technology solutions company. In Arizona, it is Zyter, Inc., a tech and AI agent company serving payers. In Ohio, it is Innovaccer, a health care data and AI company.
Preauthorization: A ‘Fix’ for a Non-Existent Problem
The stated reason behind the move to introduce preauthorization in traditional Medicare is CMS’s persistent view that overutilization of health services is what is driving costs up, despite the evidence that the driver of rising costs is the rising price of health services. A 2003 article in Health Affairs by leading health economists, “It’s the Prices, Stupid,” found US health service use was below the OECD median of peer countries. It was high prices that drove costs up. The researchers repeated the study in 2019, “It’s Still the Prices, Stupid,” and found that rising prices were still behind the increase in costs. A separate study reported in 2021, found the bulk of cost growth since 2004 was due to increased prices.Administrative costs along with excessive profits are a big part of the story of rising health care spending.
The requirement for prior authorization in MA is a main reason nearly half of eligible seniors continue to choose traditional Medicare. If retirees anticipate that they may need expensive health services as they age, they may want to avoid the hassle of deny-and-delay that is all too often associated with preauthorization requirements. CMS’s declared effort is to have all seniors in MA or in shared savings programs by 2030 that have incentives similar to MA that restrict utilization of health services. If traditional Medicare were to adopt prior authorization, it could weaken the program and accelerate the growth of MA enrollment.
There are concerns that introducing the bureaucratic preauthorization process in traditional Medicare will limit access to care and lead to worse outcomes for beneficiaries. Providers warn that this preauthorization pilot may result in inappropriate denials that prevent patients from getting care they need, add an additional layer of administration, have a difficult appeals process, and lack sufficient guardrails for use of AI in making prior authorization decisions. The American Hospital Association is calling for delaying implementation and a trial run before proceeding.
Insurance companies, for their part, welcome the WISeR model because they claim it will root out waste and avoid spending on low-value procedures that do not help patients or whose positive effects are small relative to their price. In other words, it will save them money.
This first appeared on CEPR.
The post Can the Medicare Prior Authorization Pilot Be Stopped? appeared first on CounterPunch.org.
This post was originally published on CounterPunch.org.