A coalition of humanitarian groups warned Sunday that the world could face “wave after wave of variants” unless rich countries stop blocking a proposed patent waiver for coronavirus vaccines and immediately distribute the technology needed to mass-produce the lifesaving shots.
“Business as usual has led to huge profits for pharmaceutical firms, but many people left unvaccinated means that this virus continues to mutate,” said Winnie Byanyima, executive director of UNAIDS and co-chair of the People’s Vaccine Alliance, which includes dozens of organizations spanning the globe.
“It is the definition of madness to keep doing the same thing and expect a different outcome,” Byanyima added. “We need to press reset.”
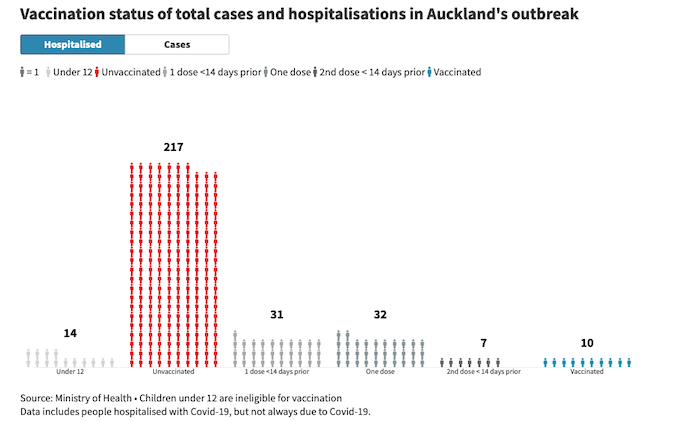
The warning from alliance members came as the recently detected and heavily mutated Omicron variant continued wreaking havoc worldwide, spreading in nearly 40 countries and fueling an alarming spike in hospitalizations among children in South Africa. First detected in southern Africa last month, the variant has since been found in nearly a third of U.S. states.
While disastrous for the global poor and vulnerable, Omicron’s rise has been a major boon for top investors in Pfizer and Moderna, U.S.-based firms that have refused to share their vaccine recipes with developing countries. Both corporations are preparing to quickly reformulate their publicly funded vaccines to combat Omicron.
“What is the point in developing new vaccines in 100 days if they are then only sold in limited amounts to the highest bidder, once again leaving poor nations at the back of the queue?” Anna Marriott, the health policy manager for Oxfam International and a spokesperson for the People’s Vaccine Alliance, asked in response to the pharmaceutical giants’ plans.
“We cannot correct the mistakes of the past 21 months,” she said, “but we need rich countries to chart a new path forward in which they step up and insist the pharmaceutical companies start sharing their science and technology with qualified manufacturers around the world, so we can vaccinate people in all countries and finally end the pandemic.”
The People’s Vaccine Alliance has long argued that the frequent emergence of new coronavirus strains is virtually inevitable as long as huge swaths of the global population remain without access to shots. Omicron is the fifth coronavirus strain that the World Health Organization has labeled a “variant of concern.”
“Fighting to buy up limited supplies of hugely expensive vaccines to protect your own citizens whilst ignoring the rest of the world will only lead to more variants, more mutations, more lockdowns, and more lives lost,” Maaza Seyoum of the People’s Vaccine Alliance Africa said in a statement Sunday.
“Pharmaceutical monopolies and profiteering have prevented vaccination in Africa and the rest of the developing world,” Seyoum continued. “It is time that pharmaceutical companies and rich nations finally put protecting people and putting an end to this pandemic ahead of profits, monopolies, and self-defeating attempts to protect themselves whilst allowing this disease to rampage across the rest of the world.”
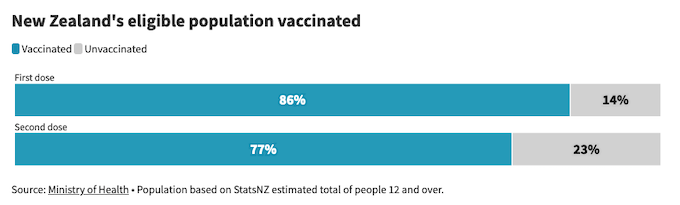
According to new Airfinity data examined by the People’s Vaccine Alliance, Sub-Saharan Africa has thus far received enough vaccine doses to fully inoculate just one in eight people while rich countries — having succeeded in getting vaccines to a majority of their populations — roll out boosters on a mass scale. A recent Financial Times analysis found that wealthy nations have administered far more boosters in four months of 2021 than low-income countries have given in total doses all year.
“It’s not only shameful that six times more booster shots are being administered daily than primary doses in low-income countries, it’s an enormous risk to ending the pandemic globally,” said John Mark Mwanika, programs officer at the Amalgamated Transport and General Workers’ Union (ATGWU-Uganda).
“It is no coincidence that the new Omicron variant was first discovered by scientists in countries which have been denied the right to produce their own vaccines,” Mwanika added. “We are in a global emergency and workers are paying the price, particularly in the Global South.”
Citing the rapid spread of Omicron, the World Trade Organization postponed its biannual Ministerial Conference late last month, prompting concerns that the body would further delay work on the proposed vaccine patent waiver. Led by India and South Africa, the measure would temporarily suspend intellectual property rules that, according to critics, have hindered global vaccine production at the expense of developing nations.
In a joint statement directed at member nations of the European Union — one of the last remaining opponents of the patent waiver — the People’s Vaccine Alliance and nearly 200 other groups argued that the current global intellectual property regime has “created an artificial supply shortage of urgently needed vaccines, tests, and treatment, leading to countless preventable deaths.”
“We call on the E.U. to stop blocking and start engaging with the TRIPS waiver proposal as presented by its co-sponsors,” the coalition said. “History will not forgive nor forget those who choose to uphold a broken system over ending the pandemic.”
This post was originally published on Latest – Truthout.