As this week marks the 20th anniversary of the September 11 attacks, we look at an enraging new documentary, 9/11’s Unsettled Dust, on the impact of the toxic, cancer-causing smoke and dust that hung over ground zero and how the Environmental Protection Agency put Wall Street’s interests before public health and told people the air was safe to breathe. One of the key figures in the film is Democracy Now! co-host Juan González, who was among the first to expose the public health and environmental crisis at ground zero in a series of reports for the New York Daily News. He says the intense backlash from the mayor’s office and federal officials “cowed” the newspaper, but he has no regrets. “My only mistake was believing that it would take 20 years for people to get sick,” González says. “It took about five years for the deaths and the severe illnesses to really become apparent.” Director Lisa Katzman says she made the film because she was a resident of Lower Manhattan who saw the attack and its aftermath up close and wanted “to address the lack of accountability” from city and federal officials. “The same people that were always touting ‘Never forget! Never forget!’ and constantly reminding us of the heroism of these responders were unwilling to do anything to actually help them,” notes Katzman.
AMY GOODMAN: We’re going to start with a warning to our listeners and viewers: Today’s show includes graphic images and descriptions, some that you may certainly have heard and seen before.
Yes, this week marks the 20th anniversary of the September 11th attacks on the World Trade Center towers in New York City and the Pentagon in Washington, D.C., that killed nearly 3,000 people. We’ll never know exactly how many people, because those who go uncounted in life go uncounted in death, perhaps the undocumented workers around the area.
But we begin our coverage looking at the impact of the toxic, cancer-causing smoke and dust that hung over ground zero in Manhattan as the fire burned for 100 more days. At the time, the Environmental Protection Agency told people who worked at the site and lived and went to school near it that the air was safe to breathe. In the years that followed, more than 13,200 first responders and survivors have been diagnosed with a variety of cancers and chronic respiratory and gastrointestinal illnesses. At least — well, close to 1,900 first responders, survivors and workers who recovered bodies and cleaned up the wreckage have since died from illnesses, many of them linked to their time at ground zero.
For the whole hour, we’re looking at an enraging new documentary that exposes the massive environmental and public health crisis caused by the 9/11 attack and how politicians and the EPA head, Christine Todd Whitman, the former governor of New Jersey, put Wall Street’s interests before public health in the aftermath. It also shows how 9/11 responders and survivors had to fight for healthcare justice while they were sick and dying, going to Washington scores of times, in wheelchairs, on crutches, with oxygen. Yes, tons of toxic dust fell on New York City 9/11. While concentrated in the 16-acre disaster site, wind carried the chemical contaminants throughout the city, in Manhattan, Brooklyn, Queens. This is the trailer for the new documentary, 9/11’s Unsettled Dust.
ONLOOKER 1: Yeah, it seemed like it just sort of —
ONLOOKER 2: Oh my god! Oh my god!
DISPATCHER: Yo, the North Tower is coming down. All units, be advised that the North Tower is coming down.
JUAN GONZÁLEZ: Once we saw the actual initial reports, we started realizing there was benzene. There was lead in the air. I was already getting warnings that there were many more potential toxic exposures.
UNIDENTIFIED: When we heard Christine Todd Whitman get on TV and say the air quality is safe, we were horrified.
CHRISTINE TODD WHITMAN: The concentrations are such that they don’t pose a health hazard. We’re going to make sure everybody is safe.
JOHN FEAL: You know, not only did we inhale and breathe in the air, we were drinking it and eating it. And I bitched and moaned to anybody who would listen to me.
REP. CAROLYN MALONEY: My husband and I and other people who were engineers went down to the site. And there was no question that it was an unhealthy site.
UNIDENTIFIED: They didn’t have a mask in the beginning, because some people were using Home Depot masks, even the guys at ground zero.
JOHN McNAMARA: On 9/11, responded, the World Trade Center, breathing in all the toxic air, and they said it was safe to breathe.
JOHN FEAL: We’re talking about human life. We’re talking about men that couldn’t be here, that had traveled with me, the 80 trips that I made to D.C., that are laying in ICU or at home with IVs in them.
JON STEWART: The first responders were told the Zadroga Act would be included — they were told this last week — it would be included in the transportation bill passed last week.
SEN. KIRSTEN GILLIBRAND: Not one of the first responders standing with me here today should have to be here today. Not one of them should have to take another trip to Washington.
JOHN FEAL: This is about Washington, D.C., helping out people from 431 congressional districts that went to ground zero. New York wasn’t attacked; this country was attacked.
AMY GOODMAN: That’s the trailer for the new documentary, 9/11’s Unsettled Dust, which premieres later this week on PBS stations in New York, New Jersey and Long Island.
For more, we’re joined by Lisa Katzman, the film’s director and producer. One of the key figures in the film is Democracy Now!’s Juan González, who is not only co-host today, but his critical work at the beginning of the time after 9/11 just changed the landscape of how people understood what was happening near and around the pile. He and Joel Kupferman of the Environmental Law & Justice Project were among the first to expose the public health and environmental crisis at ground zero in a series of reports for the New York Daily News. Juan González is also the author of the 2002 book, Fallout: The Environmental Consequences of the World Trade Center Collapse.
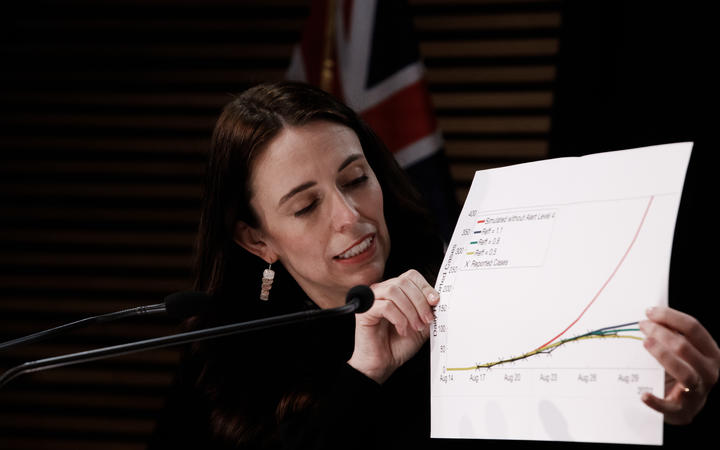
So, Juan, we’re beginning with you. I mean, that New York Daily News cover that caused so much outrage and response and attack on you, it was in October. It said “exclusive.” And we’re going to show it right here. “Toxic Zone” was the headline, “Levels of benzene, dioxin, PCBs and other dangerous chemicals at Ground Zero exceed federal standards.” That may not surprise people now, Juan, but you’re the one who had it on the cover at a time when the EPA head was telling the country all was well in Lower Manhattan in terms of safety for people returning to work. Talk about how you came to understand how toxic ground zero was.
JUAN GONZÁLEZ: Well, Amy, I actually had started — I did an article about less than three weeks after the attack on the World Trade Center, on September 28th, which began to talk about the high levels of asbestos that Joel Kupferman had discovered in his own independent testing that he had done around ground zero, even as far down as Battery Park, and very high levels of asbestos and of fiberglass, which ended up being actually responsible for much of the scarring of lungs that many of the first responders and other people downtown had. And so, I had actually done two articles before, before that big front-page story. But then, of course, as Joel was able to get even more public records requests on health testing that had been hidden from the public, that big October 26 article, as I recall, was the one that laid out those findings.
And the response was unbelievable, the backlash against it from the mayor’s office, from the EPA to the Daily News, to the point that, actually, my editors pulled back. They began, after that, beginning to hold my columns. And at one point, I actually had to go to the editor-in-chief at the time, a guy by the name of Ed Kosner, and I said, “Ed, why are you holding up my follow-ups on this?” And he says, “Well, you know, City Hall says this, and EPA says you’re overstating the problem, you’re sensationalizing. And The New York Times is not following our stories, and none of the other press are agreeing with us.” And I said to him, “Well, since when do we depend on other media to tell us how to report what we find?” So, it became clear that the paper had been cowed by the federal and the city government.
So I said to Kosner at the time — I said, “Ed, you don’t really know me. You just got here about a year ago. And I don’t know you. So this is what I’m going to do. You run the paper. You’re in charge of the paper. And I’m in charge of my column. So, I’m going to keep writing about this issue, because I don’t want it on my conscience that 20 years later people are going to start getting sick and dying because we didn’t warn them of the potential health effects here. And so, I’m not going to stop writing about this.” And the paper did end up killing some of my columns, but they ran most of them at the back of the page — at the back of the paper.
My only mistake was believing that it would take 20 years for people to get sick. It actually took far less, took about five years for the deaths and the severe illnesses to really become apparent. And by then, the paper had a new management, a new editor. And then the paper embarked — the editorial board embarked on a campaign to reveal the deaths and the illnesses that were occurring. And eventually it won the Pulitzer Prize. The Daily News won the Pulitzer Prize, the editorial board, for its coverage of the health effects, the very health effects that five years earlier it had tried to squash. You know, so, history has a strange way of evolving on issues like this. And I think that it’s a lesson that most media are very good at exposing problems far away. The closer the problems get to home, the more difficult it becomes to expose them.
AMY GOODMAN: You should have won the Pulitzer Prize for your series of prophetic reports. I wanted to go to David Newman with NYCOSH. That’s the New York Committee for Occupational Safety and Health. He’s speaking in the documentary, 9/11’s Unsettled Dust.
DAVID NEWMAN: There was substantial data available prior to the event that would indicate issues of concern with the collapse of the Twin Towers. One of those was the widely known and widely documented and widely advertised heavy use of asbestos during the construction of the World Trade Center project. So, the figure that is in widespread circulation and uncontested is that there were 400 tons of asbestos used in sprayed-on fireproofing material in the Trade Center construction. That figure excludes probable additional asbestos used in pipe insulation and other applications. So there’s a huge amount. I think it’s safe to say that whatever was in the World Trade Center was released into the general environment. Nothing disappeared.
AMY GOODMAN: “Nothing disappeared.” Whatever was inside the World Trade Towers became what we breathed. That’s David Newman with the New York Committee for Occupational Safety and Health. And, Juan, you talked about the New York Daily News winning the Pulitzer, but you didn’t, and you should have. You were the one who led the way in exposing this.
I wanted to bring in the director, Lisa Katzman, director and producer of this utterly devastating documentary, 9/11’s Unsettled Deaths [sic], 9/11’s Unsettled Dust. It could be “unsettled deaths.” And we’re going to be talking about that in a minute.
But talk about why you chose to make this film, and the significance of a crusading reporter, like Juan González, and others who were putting out this information going against the financial establishment. Let’s remember who the “country’s mayor” was at the time: Rudy Giuliani. The Environmental Protection Agency administrator, who now says, OK, maybe she made a mistake — she dreads the 9/11 anniversary because of this — Christine Todd Whitman, saying, “Everyone, back to work.”
LISA KATZMAN: Well, it’s an honor to be on the show. And hello to both of you. Hi, Juan. It was good to hear you report on those first stories that you did, again.
Yes, the reason that I was drawn to make the film is I’m a member of — I live downtown. I live four blocks from the World Trade Centers, and then what became ground zero. And I witnessed the recovery, the rescue and recovery effort, through looking through my living room windows at it over a number of months. And it was very evident — fortunately, at the time, I had a teaching job upstate, so I was not in my apartment on a full-time basis. But to anybody that lived here, who spent any time here or near downtown Manhattan, it defied one’s senses and common sense to imagine that this wasn’t a horrendously, I mean, off-the-charts environmental disaster. And so, the statement that the air is safe, the denials that were made were utterly absurd. I mean, the level of disconnect from reality is almost legendary, I would say at this point. It’s really hard to fathom that those things were said.
And the reason that I felt that I needed to make the film was to address that and to address the lack of accountability at the time. And then, what ensued, you know, in the years afterward, is that that lack of accountability traveled through the courts. It traveled through the way that Republicans in Congress thought about what should be done to help first responders. And the same people that were always touting “Never forget! Never forget!” and constantly reminding us of the heroism of these responders were unwilling to do anything to actually help them. And so, the hypocrisy of that, the rage that I felt over that as time went on, led me to want to make this film, which I began doing in 2010, when the first responders were making very — they had been making trips to D.C. to pass the James Zadroga 9/11 Health and Compensation Act for some time, but there was an intensification of those efforts in 2010, and that’s when I began filming.
AMY GOODMAN: I wanted to go to another part of the film. I mean, every three minutes, your jaw drops. This is the EPA’s Hugh Kaufman and Kimberly Flynn, founder of 9/11 Environmental Action, speaking about the EPA’s failure to warn people of the dangerous conditions at ground zero, and perhaps why.
HUGH KAUFMAN: People told us, “I’m not allowed to wear a respirator, because there are cameras around, and they don’t the optics of me wearing a respirator down here cleaning up.”
KIMBERLY FLYNN: Everyone came. Everyone who was affected came. There were responders. There were area workers. There were many, many residents and tenants’ association leaders. And there were scientists also who were bringing their information.
HUGH KAUFMAN: Christine Todd Whitman, the head of EPA, who was telling the people the air is safe to breathe, owned a quarter of a million dollars in stock from Citigroup, and her husband worked for Citigroup. Travelers insurance company had insurance policies such that if the air wasn’t safe to breathe, it could cost Travelers insurance half a billion, a billion dollars in claims. Well, guess who owns Travelers insurance: Citigroup. And that’s how the insurance companies saved billions of dollars by Christine Todd Whitman’s lie.
AMY GOODMAN: Juan, talk about the significance of this, the personal financial connections, what this meant for so many people, and continues to mean for the sick and the dying today.
JUAN GONZÁLEZ: Well, Amy, I think people should remember that Christine Todd Whitman did not act alone. She basically was acting under orders. And it was later revealed, I think by the treasury secretary under the Bush administration, that George Bush had — the president at the time had directly ordered that Wall Street be reopened within a week of the attacks, because there was a fear in the administration that the continued closing of the financial markets was going to have a disastrous effect on world capitalism.
So, basically, once Bush ordered that Wall Street be reopened — and that meant thousands and thousands of financial industry workers had to come back to downtown Manhattan — then the health officials, including Christine Todd Whitman, had to justify, had to justify the orders. And rather than do the science first and then figure out what the policy, the policy was established, and the science was made to fit the facts.
It was later revealed by the EPA’s inspector general report that the White House — the head of the environmental policy at the White House, a guy by the name James Connaughton, had actually rewritten the press releases that the EPA was putting out, to downplay the health impacts. So this was a direct order from the White House to get Wall Street back up and running, and the rest of the population of Lower Manhattan basically, in essence, were collateral damage to that policy.
AMY GOODMAN: This is President George W. Bush’s EPA Administrator Christine Todd Whitman testifying at a 2007 congressional hearing on whether the federal government’s actions at the 9/11 attack sites, at the pile, violated the rights of first responders and local residents.
CHRISTINE TODD WHITMAN: I got a call from the White House a day after, from the Office of the Economic Adviser, which is not surprising — they’re concerned about the economy of the country — saying — reminding me of the importance of Wall Street, of opening the stock market. I indicated that until that building was cleaned, until it was safe, it would be inappropriate. And that’s the last I heard of that. It was cleaned. It was safe, as you have heard from Mr. Henshaw, for them to go back in. And they were allowed back in. Was it wrong to try to get the city back on its feet as quickly as possible, in the safest way possible? Absolutely not. Safety was first and foremost, but we weren’t going to let the terrorists win.
AMY GOODMAN: “We weren’t going to let the terrorists win.” During the hearing, Whitman was questioned by Florida Democratic Congressmember Debbie Wasserman Schultz.
REP. DEBBIE WASSERMAN SCHULTZ: The EPA does have the — did have the ability to take over the site at the point that they felt that — and that is under Presidential Decision Directive 62, Emergency Support Function 10, and the National Contingency Plan under CERCLA. The EPA could have taken over control of the site from the city as the lead agency, if they felt that the city was not properly protecting their workers. So they certainly had the ability to do it, and you chose not to. So, if you are saying that the law wasn’t structured in New York to allow you to do that, then why didn’t EPA step in and take over?
CHRISTINE TODD WHITMAN: Congresswoman, under — as you know, EPA would have, under certain circumstances, had the authority to take over the site. What had to be proven in order to invoke the CERCLA, or the Superfund Act, substantive, substantial and imminent danger. And the readings that we were getting, relative — and this was relative to the overall air; I’m talking more about outside of the pile — were not indicating that. And we were working in a collegial fashion with the city of New York. Again, as far as the workers on the pile, what our — we were tasked by OSHA to do the — I mean, excuse me, by FEMA to do the health and safety monitoring, to monitor the air. And we did that, and then we provided as many respirators —
REP. DEBBIE WASSERMAN SCHULTZ: But, you know, when it comes to —
CHRISTINE TODD WHITMAN: We were not tasked with —
REP. DEBBIE WASSERMAN SCHULTZ: — to imminent — substantial and imminent danger, are you talking about immediate death, horrible sickness within weeks? Because mesothelioma, the cancer that is —
CHRISTINE TODD WHITMAN: Right.
REP. DEBBIE WASSERMAN SCHULTZ: — that is the result of exposure to asbestos, does not manifest itself substantially or immediately. It could be years. But it’s almost certain. So, how is it that you didn’t step in and exercise your authority, given that knowledge, which has been known for years?
REP. JERROLD NADLER: The gentleman — the gentlelady’s time is expired. The witness may answer the question.
CHRISTINE TODD WHITMAN: Congresswoman, that was based on what the interpretation of what our legal ability was to act by — in consultation with counsel at the time.
AMY GOODMAN: And that was Jerry Nadler, New York congressmember, who represented the ground zero area, chairing the meeting, Christine Todd Whitman being questioned by Florida Democratic Congressmember Debbie Wasserman Schultz. Before we go to break and then hear the story of Joe Zadroga — you may think you know it, because his name is on the law, but I don’t think you know the details. Juan, your comment on what Christine Todd Whitman was saying and the information that was being suppressed from the highest levels? Nadler would go on to say that she and “America’s mayor,” Mayor Giuliani, should be tried for criminally negligent — for criminal negligence.
JUAN GONZÁLEZ: Well, I think it’s important to recall the role of Rudy Giuliani, as well, because, you see, the EPA was a monitoring agency. The federal agency that should have assured the protection of all the people at ground zero was OSHA, the Occupational Safety and Health Administration. And OSHA deliberately did not enforce its standards for working on a dangerous site like that, because Giuliani insisted that he was in charge. He was the incident commander on the pile, and he kept — he maintained his control of all information and all activity at the pile long after what should have been just a rescue operation. So, therefore, OSHA was not allowed by Mayor Giuliani to actually conduct its legally required business. And as a result, many, many people ended up being exposed and getting sick and not having proper protection. And we should never forget the role of Rudy Giuliani in allowing that situation to go on for so long.
AMY GOODMAN: And that was very different at the Pentagon, which was also attacked, where they had the proper attire. We’re going to talk with Joe Zadroga in a minute. The bill is the James Zadroga Act, his son, who has since died. Stay with us.
[break]
AMY GOODMAN: “A Hunting We Will Go,” performed by The O’Neill Brothers. It was sung by Michael Williams in The Wire, well known for that, Michael Williams who has died at the age of 54 in Brooklyn.