By Christine Rovoi, RNZ Pacific journalist
The government-designed vaccination rollout in New Zealand has not mobilised Pacific communities to respond safely and effectively, the Pacific Leadership Forum said.
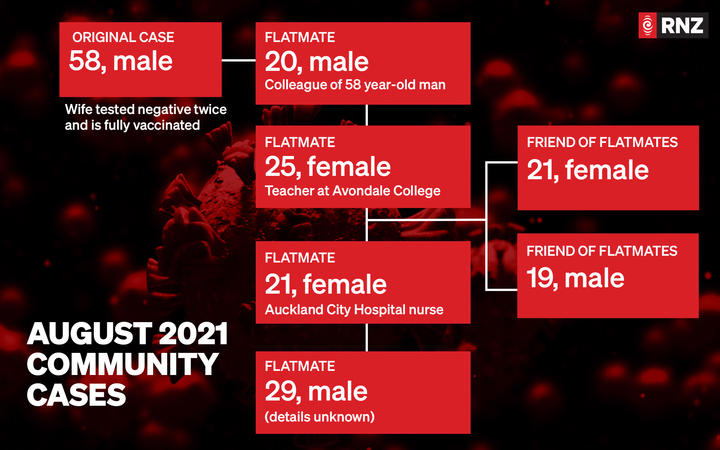
More than 50 percent of covid-19 infections in New Zealand are of Pacific descent.
But they have one of the lowest vaccination rates in the country.
- READ MORE: 41 new covid cases in New Zealand community, says Bloomfield
- Other NZ covid lockdown reports
- LISTEN TO RNZ CHECKPOINT: Call for change to Pasifika strategy (duration 3:04
Pakilau o Aotearoa Manase Lua is chair of the Pacific Response Coordination Team (PRCT) and said this showed the current vaccination strategies were not working for Pacific peoples.
The Tongan community leader said this was despite millions of dollars being allocated towards covid-19 vaccination stations, communications and PR companies to drive awareness and engagement.
“I don’t blame our communities at all. A lot of them are hearing a lot of misinformation through social media on the vaccines,” he said.
“There’s uncertainty because now they hear that their children don’t even need permission. It’s all on the Ministry of Health’s website. Children who want to get vaccinated don’t need to tell their parents.”
PRCT helped mobilise Pacific communities
Pakilau said during last year’s outbreak in April, the PRCT helped mobilise Pacific communities to get tested at the Ōtara South Seas, when Pacific testing was low.
In August, the PRCT and other Pacific providers set up a pop-up community testing station at a Māngere church, “when a government response was not forthcoming”, he said.
“That’s not going to help our communities feel safe. They want to know what’s going on,” Pakilau said.
“It just feels like the government, DHBs and the officials are forgetting the community, and forgetting to communicate with us. Come and talk to us. The biggest problem is they are not willing to listen to Pacific voices.”

One location of interest in this latest outbreak is the Samoa Assemblies of God Church in the south Auckland suburb of Māngere.
Reverend Victor Pouesi is the minister at the EFKS Puaseisei Magele Sasa’e – Māngere East Congregational Christian Church of Samoa.
He said the church was one of the clusters in last year’s outbreak and some people are still confused about the “whole vaccination thing”.
Engaging church, community
He said the government should have engaged the church and community leaders in their response efforts.
“Now it shows in this vaccination campaign, people feel more comfortable coming to church and getting vaccinated especially our Pacific people because that’s where they go for comfort, for spiritual nourishment and this is where they always meet,” he said.
“If we are not able to get together and be a part of this response effort, things will get out of hand. Our people are already panicking, most of them fearing the worst.”
Minister for Pacific Peoples ‘Aupito William Sio says more Pacific providers are needed and work is continuing on the roll out in Pacific communities.
Aupito also said church leaders should advise their congregations to get tested, after it was revealed an infected person attended Sunday service.
“We’re not blaming anybody other than the virus. But we really do need the cooperation of our church leaders, particularly when there is a positive test in and among your congregation.”
‘Aupito was adamant Pasifika will not be judged based on their ethnicity.
Strategy worries health experts
Two Pacific clinical health experts and members of the government’s covid-19 response teams have expressed their concerns about the effectiveness of the strategies.
Dr Collin Tukuitonga said the DHB’s mass vaccination event held in Mānukau, earlier this month, was ineffective in reaching Māori and Pacific communities.
Dr Api Talemaitoga said “the event lacked Māori and Pasifika input”.
“Current vaccination rollout strategies are highly top-down in approach and lack authentic Pacific community dialogue or initiative,” he said.
“There have been some positive gains in information dissemination, however they have failed to mobilise Pacific communities to be vaccinated.”

Pakilau said that to increase Pacific vaccination numbers a “by community for community approach” was required — “that is a bottom-up approach.”
“Pacific communities are at risk during the rising pandemic, and we must take community action.
Top-down continues inequitable outcomes
“The government rhetoric and top-down approach imposed on our communities continues inequitable outcomes.
“To increase vaccination uptake for Pacific communities, a truly community designed, partnered approach that is resourced is required to equip and empower our leaders to mobilise their communities across the nation.
“Pacific people stand with Māori when they fervently said ‘He tangata, he tangata, he tangata’. It is the people, it is the people, it is the people.”
The Pacific Response to Covid-19 Team is a committee of the Pacific Leadership Forum and represents up to 10 Pacific ethnic groups from across the country.
It was established in March 2020 to provide a community response to the pandemic.
This article is republished under a community partnership agreement with RNZ.
This post was originally published on Asia Pacific Report.