Respon pemerintah daerah dan masyarakat sipil terhadap pandemi Covid-19 di Indonesia telah banyak dipuji dalam media akademis dan populer sejak kasus pertama Covid-19 dikonfirmasi Maret 2020. Mitigasi lokal dan respon kesehatan telah terbukti menjadi faktor kritikal ketika pemerintah pusat telah gagal dalam banyak aspek penanganan pandemi. Namun apa yang tidak ditunjukkan oleh kajian-kajian awal adalah peran yang dimainkan kaum perempuan dalam memimpin tanggapan lokal ini. Kajian baru saya mengungkap kesenjangan antara keterwakilan tinggi kaum laki-laki dalam kepemimpinan formal dan badan pengambilan keputusan tanggap COVID-19 di satu sisi, dan dominasi perempuan yang luar biasa dalam kepemimpinan sehari-hari baik dalam mitigasi maupun perawatan kesehatan. Meskipun saya hanya berfokus pada satu kota di Jawa Tengah, kita dapat berasumsi bahwa fenomena ini juga terjadi di bagian lain Indonesia dan di banyak bagian dunia.
Hasil penelitian yang diterbitkan dalam laporan baru saya, menjelaskan kenapa keterwakilan perempuan dalam struktur satuan tugas (Satgas) Covid-19 sangat minimal, sementara di sisi lain mereka mendominasi peran garis depan baik tanggap darurat maupun penanganan pandemi jangka panjang. Pada bulan Januari dan Februari 2021 saya melakukan penelitian lapangan dengan seorang mahasiswa paska sarjana di kota Salatiga, Jawa Tengah. Kami mengumpulkan data tentang peran kepemimpinan Aparat Sipil Negara perempuan dalam penanganan pandemi. Dalam kajian ini saya memperluas penelitian saya sebelumnya tentang respon pandemi di tingkat lokal, dengan menerapkan lensa gender untuk memeriksa mengapa pejabat dan petugas kesehatan perempuan, yang memiliki peran dan tanggung jawab terbatas pada Satgas Covid-19 kota dan kecamatan, dalam prakteknya telah menjalankan peran kritikal dalam memimpin strategi mitigasi di kedua tingkat tersebut.
Tembol dibawa untuk mengunduh dokumen arahan kebijakan seluruhnya.
Kegagalan struktur satuan tugas COVID-19 di tingkat lokal
Peraturan nasional menyatakan bahwa kebijakan pengarusutamaan gender harus diintegrasikan dalam rencana tanggap darurat dan bencana baik di tingkat nasional maupun di bawahnya. Kenyataannya, keterwakilan kaum perempuan di Satgas Nasional hanya 7%, serta 12% untuk Satgas Provinsi Jawa Tengah. Sejak bulan Februari 2020, pembuatan kebijakan penanganan pandemi tingkat nasional sama sekali tidak membuat ketentuan terkait dengan gender. Dalam komposisi pegawai pemerintahan Kota Salatiga, tingkat perimbangan keterwakilan secara gender lebih tinggi dari rata-rata nasional, namun perempuan yang menduduki jabatan eselon tinggi masih sangat sedikit. Kesenjangan ini, pada gilirannya memberikan dampak langsung pada penyusunan anggota Satgas COVID-19 Kota Salatiga, dimana posisi-posisi di dalamnya dialokasikan atas dasar jabatan struktural dalam pemerintahan, tanpa mempunyai rujukan khusus pada gender.
Dalam struktur anggota Satgas yang disusun bulan Okober 2020, partisipasi perempuan hanya 17% dari sebuah tim beranggotakan 12 orang. Kepala-kepala instansi pemerintah yang strategis, Kepolisian Resor (Polres), Komando Resor Militer (Korem), Satuan Polisi Pamong Praja (Satpol PP), Badan Perencanaan Pembangunan Daerah (Bappeda) dan kantor Kesatuan Bangsa dan Politik (Kesbangpol), secara otomatis ditunjuk untuk masuk dalam struktur Satgas, dan semua posisi ini dijabat oleh laki-laki. Meskipun melanggar prinsip pengarusutamaan gender, gambaran lokal dari Kota Salatiga ini adalah keadaan tipikal di seluruh Indonesia baik di wilayah jabatan publik yang diduduki lewat pemilihan maupun karir kepegawaian, dengan laki-laki adalah mayoritas pemegang jabatan eselon tinggi.

Rapid Test facility at Pasar Senen Station. Image credit: Gaudi Renanda in Wikimedia Commons Creative Commons Attribution-Share Alike 4.0
Satgas COVID-19 Kota Salatiga bertanggung jawab dalam hal kebijakan dan perencanaan strategis mitigasi pandemi, koordinasi lintas instansi, pemantauan dan penegakan langkah-langkah mitigasi, alokasi anggaran dan sumber daya lainnya. Terlepas dari peran kepemimpinan yang tersemat pada lembaga yang didominasi laki-laki ini, dalam prakteknya kaum perempuanlah yang secara prinsip telah memimpin tindakan mitigasi dan penanganan kesehatan. Para perempuan ini telah berinisiatif maju untuk mengisi celah-celah kekosongan dalam kepemimpinan formal respon pandemi COVID-19, yang tidak responsif.
Peran kepemimpinan perempuan dalam pandemi
Kontras dibanding struktur Satgas COVID-19 tingkat kota, Dinas Kesehatan Kota Salatiga memiliki proporsi perempuan yang jauh lebih tinggi baik dalam peran kepemimpinan maupun tenaga kesehatan lapangan, dimana kaum perempuan mencakup 80% dari seluruh pegawainya. Di tingkat komunitas, kerja-kerja penangangan COVID-19 lebih lagi didominasi oleh kaum perempuan. Kepala dari enam Puskesmas di Kota Salatiga semua adalah perempuan, dengan 90% tenaga kerja adalah perempuan.
Secara praktis, aspek penanganan pandemi ini tak hanya pelayanan kesehatan, namun juga meliputi wilayah-wilayah kritikal lain terkait mitigasi penyakit menular, yang dipimpin oleh kaum perempuan dari Dinas Kesehatan, Puskesmas dan dari pusat perawatan di rumah sakit daerah dan rumah sakit lain di Salatiga. Kelemahan utama penanganan pandemi yang telah diidentifikasi oleh semua responden dalam wawancara adalah kegagalan Satgas untuk memberikan kepemimpinan dan arah. Seorang pejabat Dinas Kesehatan menyampaikan bahwa meskipun terdapat instansi-instansi pemerintah yang mempunyai tanggung jawab sendiri-sendiri dalam Satgas, dalam prakteknya, mereka selalu lari ke Dinas Kesehatan untuk mendapatkan pemecahan masalah.
Perempuan yang memimpin di pusat kesehatan kota dan kecamatan berpendapat bahwa penguatan peran Satgas tingkat kota sangat perlu, untuk: secara efektif melakukan pengawasan dan penilaian pelaksanaan kebijakan di lapangan, serta mensupervisi komunikasi publik yang efektif, termasuk mengkomunikasikan kebijakan mitigasi, sehingga layanan kesehatan dapat memprioritaskan diri pada pendalaman pengetahuan mengenai berbagai ilmu terkait COVID-19 yang berkembang sangat cepat dan dinamis, serta ilmu penanganan pandemi.

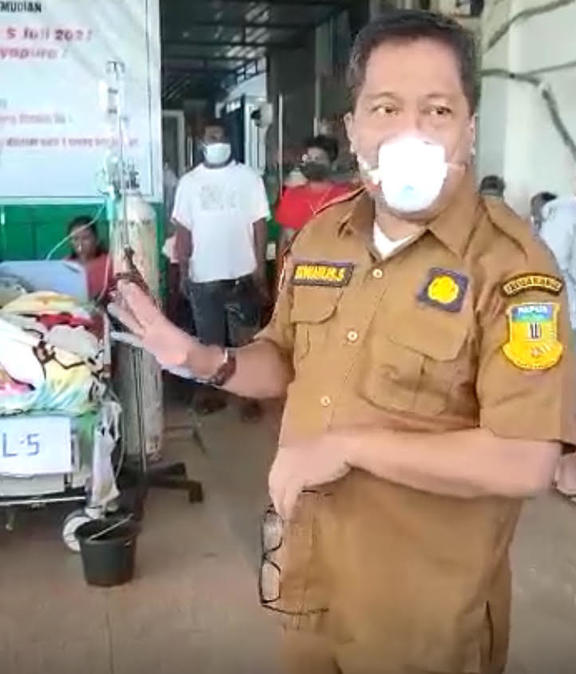
Sebuah spanduk yang menyampaikan strategi mitigasi untuk COVID-19. Dipotret oleh penulis.
Laporan saya menunjukkan bahwa ada empat institusi yang sangat penting dalam pelayanan kesehatan garis depan; Dinas Kesehatan, Puskesmas, rumah sakit daerah dan fasilitas isolasi khusus. Dua lembaga yang disebut pertama juga punya peranan vital dalam pelaksanaan mitigasi. Dan Puskesmas adalah tulang punggung dari strategi mitigasi dan perawatan kesehatan sebagai garis depan pelaksanaan pengetesan, penelusuran dan dukungan pada mereka yang terinfeksi COVID-19.
Respon-respon strategis dari layanan kesehatan ini inovatif; secara cepat melakukan reorganisasi tenaga kesehatan dan penyesuaian tugas-tugas. Terdapat dua tim; yang didedikasikan untuk penanganan COVID-19, dan tim yang memastikan layanan kesehatan umum tetap berjalan.
Di tingkat masyarakat, kepala Puskesmas memprakarsai komunikasi lintas sektor antar pemangku kepentingan di wilayah kecamatan (pemerintah kecamatan, satuan polisi dan tentara setempat, serta aparat kelurahan), serta melakukan koordinasi antar elemen masyarakat, organisasi sipil, kelompok agama dan pemerintah kecamatan.
Beban kerja pandemi bagi perempuan
Kegagalan kebijakan nasional penanganan pandemi COVID-19 di Indonesia dan banyak negara lain telah meningkatkan beban kerja dari tenaga kerja kesehatan perempuan, baik beban kerja yang dibayar maupun tidak. Sebagian besar tenaga kesehatan perempuan bahkan tidak diperhitungkan, apalagi dianggap penting dalam penyusunan kebijakan publik, baik dalam hal biaya yang dialokasikan pada sektor kesehatan khususnya maupun untuk sektor-sektor sosial secara lebih umum – yang keduanya didominasi perempuan, juga dalam hal manfaat-manfaat yang diberikan kaum perempuan dalam sektor kerja pelayanan dan reproduksi sosial. Akibatnya, penangan pandemi menjadi lebih rumit dengan beban kerja yang lebih tinggi bagi perempuan di garis depan. Apalagi, tak ada tambahan sumber daya manusia, sementara perempuan-perempuan ini juga harus lebih intensif menangani implikasi pandemi dalam peran domestiknya.

Pekerja laboratori di pabrik BioFarma, Bandung, sedang memeriksa vial vaksin (bukan vaksin COVID-19). Image credit: Ümit Kartoğlu for VOA on Wikimedia Commons (public domain).
Penting sekali untuk dicatat bahwa para perempuan ini telah mengembangkan pengetahuan secara signifikan melalui pengalaman mereka menangani pandemi. Mereka paham betul apa itu pandemi COVID-19 dan tahu langkah-langkah penanganan seperti apa yang bisa berjalan untuk mitigasi krisis – dan mana yang tidak. Namun terbatasnya keterlibatan perempuan dalam struktur formal yang memiliki kewenangan membuat kebijakan, telah membatasi ruang perempuan baik untuk mengkritik maupun untuk mengarahkan pembuatan kebijakan politis mengenai prioritas-prioritas dalam penanganan COVID-19.
Kontribusi perempuan pada kepemimpinan pandemi
Akademisi dan pegiat advokasi telah mendorong untuk dibukanya ruang partisipasi perempuan dalam penyusunan rancangan, pelaksanaan dan pengawasan aturan serta kebijakan terkait penanganan COVID-19 di semua tingkat pembuatan keputusan di pemerintahan. Kajian saya menunjukkan bahwa partisipasi ini sangat perlu, tak hanya untuk memastikan bahwa kebutuhan khusus bagi perempuan selama pandemi bisa terakomodasi, lebih jauh lagi, untuk bisa mendayagunakan pengetahuan yang terus berkembang serta pengalaman-pengalaman dari para perempuan ini sebagai sumber penting dalam rangka menyusun strategi-strategi penanganan pandemi yang tepat.
Manajer kesehatan dan tenaga kesehatan garis depan telah mengidentifikasi beberapa bidang yang memerlukan tindakan serius dan segera. Pertama, perlu ada koordinasi, kepemimpinan dan pelaksanaan tugas resmi yang lebih efektif di Satgas Kota. Kedua, peningkatan pemantauan dan penegakan protokol kesehatan di tempat kerja, ruang publik dan acara-acara umun yang disetujui, termasuk pernikahan, upacara dan di tempat-tempat yang memfasilitasi pertemuan publik. Ketiga, harus ada pemantauan dan penegakan aturan pembatasan pergerakan dan peraturan daerah tentang kuota work from home, pembatasan kapasitas di restoran, hotel dan tempat lainnya serta isolasi mandiri di rumah. Keempat, perlu memperbesar kemampuan penelusuran dan pengetesan, yang dicapai dengan menambah fasilitas fisik untuk mendukung pengetesan sebagai ujung tombak pemantauan epidemiologis yang baik terhadap tingkat persebaran virus. Pemantauan epidemiologi ini akan mendukung penyusunan arah kebijakan menuju penekanan pandemi COVID-19 secara lebih efektif.
Puskesmas di Indonesia, yang sebagian besar dijalankan oleh perempuan, telah menjadi bagian kritikal dari infrastruktur untuk penanganan pandemi di Indonesia. Upaya menjalin hubungan secara intensif dengan masyarakat yang dilakukan petugas-petugas Puskesmas telah menghasilkan pemahaman yang lebih besar tentang apa itu COVID-19 di masyarakat setempat, mendorong koordinasi pemangku kepentingan lintas sektor jika memungkinkan, memberikan dukungan aktif untuk pasien positif, dan mengurangi stigmatisasi masyarakat. Sayangnya, peran kritikal serta pengetahuan dan pengalaman yang diperoleh kaum perempuan ini, belum diakui secara formal ataupun dijadikan sebagai sumber rujukan penting dalam perencanaan dan kepemimpinan pandemi jangka panjang. Pada akhirnya, kegagalan ini melemahkan kapasitas untuk memberikan respon menyeluruh yang terkoordinasi dengan baik terhadap pandemi COVID-19 di tingkat lokal, yang mengakibatkan tingginya tingkat penularan virus.
Terakhir, peminggiran struktural terhadap perempuan dan kegagalan untuk mengakui pengalaman, pengetahuan dan kapasitas kepemimpinan mereka dalam penyusunan kebijakan pandemi serta pengalokasian sumber daya, secara efektif telah memperpanjang jangka waktu krisis multi dimensi yang diakibatkan oleh pandemi COVID-19.
The post Kaum perempuan di garis depan: Peran kepemimpinan yang tak dihitung dalam penanganan COVID-19 appeared first on New Mandala.
This post was originally published on New Mandala.





 Starting today at the Vodafone Events Centre in Manukau City. Our first mass vaccination event will vaccinate more than 15,000 people over the next 3 days.
Starting today at the Vodafone Events Centre in Manukau City. Our first mass vaccination event will vaccinate more than 15,000 people over the next 3 days. 



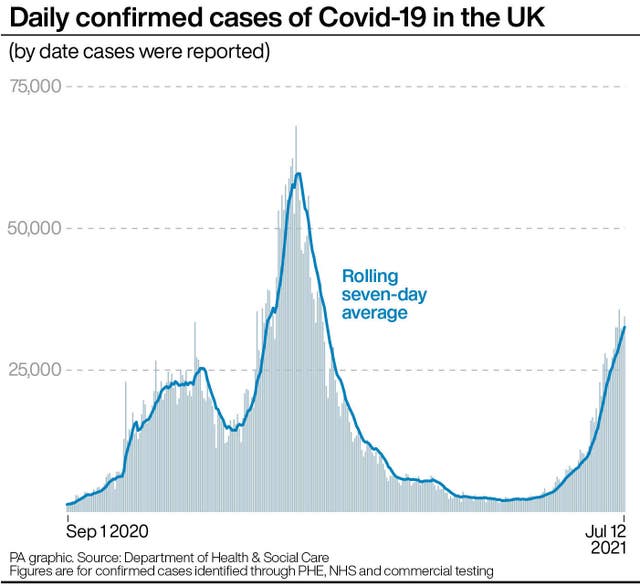
 from May) is promising but not fast enough.
from May) is promising but not fast enough.